Click the image below to read our SafER Space framework and implementation toolkit:
THIS IS AN EMERGENCY
THE TIME FOR ACTION IS NOW
Canada has one of the highest child and youth suicide mortality rates among all countries that are members of the Organization for Economic Cooperation and Development (OECD),[1] indicating children and youths in Canada are vulnerable to mental health distress. Despite this vulnerability, publicly available mental health services for children and youths are chronically underfunded and oversubscribed, leading to long wait times.
Increasingly, parents / caregivers turn to emergency rooms (ERs) to support their children and youths who are experiencing a mental health crisis, which has compounded during the pandemic – making ERs often the first point of contact families have while trying to access mental health supports. Sadly, the risk of suicide increases more than double after a young person has had an adverse ER experience related to their mental health.[2]
In response to this emergency, Myles Ahead’s flagship initiative, SafER Space, was developed. We are at a critical crossroads where children and youths need mental health supports at a time when Canada’s ERs are in crisis themselves. Fortunately, SafER Space’s framework consists of a unique phased approach that includes low-cost and easily implementable components that can be readily adapted to any ER setting, its needs, community profile, and planning processes. SafER Space is designed to actualize a strong, integrated crisis support system.
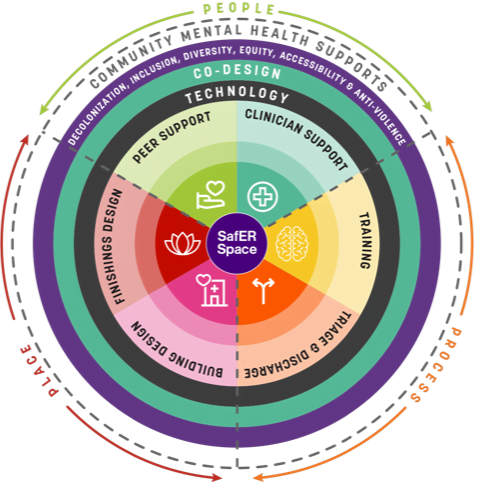
SafER Space also has immense potential to improve the workplace environment for ER employees, leveraging non-clinical peer support workers and including therapeutic elements specifically designed to facilitate de-escalation and crisis recovery. SafER Space’s evidence-informed scalable framework, as shown in the diagram below, is the result of a comprehensive global literature review, consultative and co-design process, informed by families and young people with lived experience, as well as leading experts and clinicians in Canada, the United States, and Australia.
The Framework adapts and extends existing ‘safe space’ crisis support service models from the United Kingdom, Australia, and the United States that have shown to make a real difference in the lives of families and young people, reducing suicide crises, and preventing lengthy hospital admissions, emergency wait times, and re-presentations to the ER. Initiatives that include similar components show:
- 35% reduction in ER visits and 6% reduction in 30-day readmissions when Peer Support Workers are included in ERs[3]
- Reduced physical restraints use on patients to less than 1% in hospitals that implemented EmPATH (Emergency Psychiatric
Assessment, Treatment, and Healing) units[4] - 70% decrease in hospitalizations when using an empathic model of care[5]
SafER Space intentionally and holistically reimagines ERs in their approach with young people turning to the ER while experiencing mental health distress. Designed for young people, SafER Space is the first of its kind to address this age gap. This framework provides timely and brief clinical and peer support in a comfortable, therapeutic, and calm environment that facilitates recovery, wellbeing, and safety, helping to ensure that young people, including their families, are supported in ‘stepping down’ from brief crisis intervention with adequate community links, strategies, and tools.
With your support, SafER Space’s framework can be rolled out to every ER across Canada, to help keep children and youths safe, in addition to supporting them on their path to wellness and recovery. To help spread the message, click here to access SafER Space’s press release, social media kit, and a one-click letter to write to your local MP for their support.
[1] “International Suicide Rates of Youth 15 to 24 Years of Age, Canada and Other OECD Countries – the Health of Canada’s Children and Youth.” The Health of Canada’s Children and Youth, A CICH Profile, (2012), https://cichprofile.ca/module/1/section/5/ page/international-suicide-rates-of-youth-15-to-24-years-of-age-canada-and-other-oecd-countries
[2] Gardner, William, et al. “Health Outcomes Associated with Emergency Department Visits by Adolescents for Self-Harm: A Propensity-Matched Cohort Study.” CMAJ 191.44 (2019): E1207-E1216. https://doi.org/10.1503/cmaj.190188.
[3] Kaur, M., & Melville Jr, R. H. “Emergency Department Peer Support Specialist Program.” Psychiatric Services, 72.2 (2021): 230-230, https://ps.psychiatryonline.org/doi/10.1176/appi.ps.72102.
[4] Zeller, Scott. “EmPATH Units as a Solution for ED Psychiatric Patient Boarding.” Psychiatry Advisor, 2018, www.psychiatryadvisor.com/home/practice-management/empath-units-as-a-solution-for-ed-psychiatric-patient-boarding/
[5] Brown, Denise. “EmPATH: Stopping the Dehumanization of Behavioural Health Patients in Emergency Departments.” STAT, 2 July 2019, https://www.statnews.com/2019/07/02/empath-model-behavioral-health-emergency-departments